Oral contraceptive pills (OCP) are commonly used throughout the
world. These pills contain different compositions of estrogen and progesterone.
Many side effects of OCP have been reported in literature. Ophthalmological
adverse events are no exceptions. In one study, the incidence of ocular side
effects was reported to be 1 in 230,0001. Thromboembolic conditions
associated with OCP can lead to retinal artery occlusion and
neuro-ophthalmologic consequences can occur secondary to Cerebro-vascular
accidents2. Ophthalmic migraine and intolerance to contact lenses
are also reported in literature3. The risk of complications increases
in smokers and in women older than 35 years. Primary open angle glaucoma and
raised intra ocular pressures are also known side effects of OCP, when used for
longer duration. It was reported by Wang et al that women taking OCP for more
than three years had a two-fold increase in the risk of developing glaucoma4.
However, in a recent study, it was found that OCP cause an increase in the
central corneal thickness, which could be responsible for the higher intra
ocular pressure readings in these patients5. Contrary to the
increased risk of developing glaucoma with OCP, Newmann Casey et al have shown
the protective effect of female sex hormones by decreasing intra ocular
pressure in post-menopausal women taking hormone replacement therapy6,7.
Rationale of our study is to find out whether OCP are safe to use
for a short period of time. We included subjects who had taken OCP for more
than six months and less than 3 years. Paradoxical effect of female sex
hormones in decreasing IOP is also discussed. The purpose of our study was to determine the
effect of short-term oral contraceptive pills (OCP) on intra ocular pressure of
women of childbearing age.
MATERIAL AND METHODS
The study was
conducted at Arif memorial teaching hospital and Allied hospital Faisalabad from
October 2017 to March 2018. It was a comparative observational study. Sample
was collected using non-probability convenience sampling. One hundred female
subjects were divided into two groups of 50 each. Group A, included females of
childbearing age, who had been taking oral contraceptive pills for more than 6
and less than 36 months. Group B included 50 age-matched controls who had never
used OCP.
Inclusion
criteria for the subjects were non diabetic and non-hypertensive healthy
females, taking OCP for at least six months and not more than 3 years and for controls
were non diabetic and non-hypertensive age-matched females who had never taken
OCP. The following subjects were excluded from the study: females having any
systemic and ocular disease, females with moderate to high refractive errors
(≥ +2 hypermetropia and ≥ -2 myopia), post-menopausal women and
girls of pre-pubertal age, subjects using any ocular or systemic drugs which
might affect intra ocular pressures, and subjects with history of any blunt or
penetrating ocular trauma.
Study Instruments
were Proforma, Slit lamp Bio-microscope, Applanation Tonometer and Ophthalmoscope.
Verbal informed consent was taken from the participants. History included
special emphasis on systemic and ocular diseases, use of topical or systemic
drugs and use of OCP. Careful Slit lamp examination was performed and
intraocular pressures were measured using Goldman Applanation tonometer. Fundus
examination was done to rule out any posterior segment disease. Data was
recorded on specially designed proforma. Statistical analysis was done using
ANOVA with SPSS version 21. Significance was set at (p < 0.05).
RESULTS
The average age of the patients was 29.16 years in group A and
27.74 years in group B. Average duration of using OCP was 14.9 months. The mean
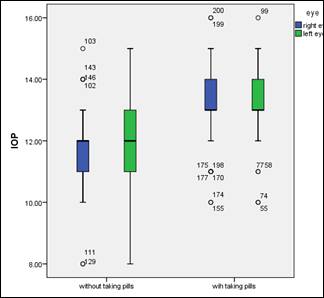
and standard distribution of IOP in the 2 groups is shown in table 1 and their
distribution is shown in box and whisker plot is shown in graph 1. There was a
significant difference between the IOP of both groups p = 0.000. Average Cup to
Disc ratio was 0.29 in group A and 0.27 in group B and the difference was not
significant (p = 0.109).
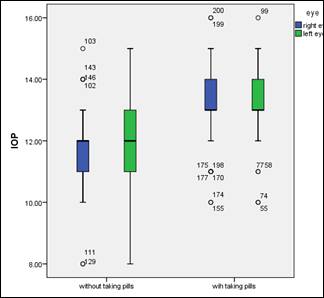
Graph 1: Showing a box-whisker plot indicating
distribution of IOP in both eyes of group A (taking OCP) and group B (without
OCP).
DISCUSSION
Intra ocular pressure is the only
modifiable risk factor in primary open angle glaucoma (POAG). Different studies
have shown contrasting results regarding the effect of OCP/female sex hormones
(estrogen and progesterone) on IOP. There are also some studies, that showed the influence
of female reproductive health on incidence of glaucoma8. American Academy of Ophthalmology (AAO)
2013 Annual Meeting reported that women using OCP for more than three years had
two folds increased risk of developing glaucoma3. Later, similar
reports were published showing that women using OCP for more than five years had a 25
percent increased risk of POAG9,10,11. Our results showed that women
using OCP for even less than three years had significantly raised IOP when
compared with controls. Although the intra ocular pressures in our study were
in the normal range and there was no significant difference in Cup to Disc
ratio, yet these pressures may have detrimental effects on susceptible optic
discs.
This contradicts the protective role of estrogens
as found in other studies. According to Blue Mountain Study, women who had less
exposure to estrogen in their lifetime were more prone to develop Glaucoma12.
It was shown that there was a 2-fold increased risk of POAG in women who had
late age of menarche and early menopause before 45 years. Hence decreasing the
exposure of estrogen to body tissues including optic nerve and retinal ganglion
cells, which become more susceptible to damage. Similar
results were shown by Nurses’ Health study by Pasquale LR9.
It was further supported by Vajaranant
TS, who explained that estrogen deficient states lead to accelerated
aging of the optic nerve hence making it more prone to glaucomatous damage13.
This effect was explained by another research,
which proved that estrogen-deprived optic nerve becomes more susceptible to
mechanical stress caused by high IOP14.
It is a known fact that age related thinning of RNFL occurs by
approximately 0.2% or 0.2 μm per year15,16.
Estrogen deprived optic nerve undergoes early aging changes making the optic
nerve more prone to glaucomatous damage. Increased IOP with OCP and decreased
with endogenous estrogen can be explained by the different chemical structure of
endogenous hormones from the OCP. Further studies are needed to prove this.
Another
possibility of increased IOP with OCP can be explained by the fact that OCP
results in decrease in the levels of normal estrogen which is considered to
have a protective effect in glaucoma. This was further supported by Bayard’s
work, according to which, the normal circadian rhythm of estrogen is lost with
OCP. This results in a false effect of deficient estrogen state17.
Another explanation of increase in IOP with OCP could be the increase in
central corneal thickness (CCT) with estrogen use18. According to
one study, IOP was increased around ovulation after the estrogen peaks19.
OCP may have the same effect on the CCT, which might have given false
impression of raised IOP. However, aging of optic nerve is also proposed as a
cause of increased incidence of glaucoma in post-menopausal women20.
The strength and importance of our study
is that we have considered short duration of OCP, which was not addressed in
earlier research works. This can be considered a pilot study and more
elaborative inquest with multivariate analysis including the effect of OCP on
CCT, IOP, RNFL and visual fields needs to be done. Limitations of our study
were that no particular composition of OCP was studied. Different results in
different studies might be due to variety of salts and combinations used in
OCP. We also did not take into account CCT, OCT and Retinal Nerve Fiber Layer
thickness.
CONCLUSION
OCP significantly increase IOP even when used for short time
period. Women who are prone to develop POAG because of positive family history,
advancing age, diabetes, myopia and smoking should have baseline tests of
glaucoma before commencing OCP. These tests should be followed up on regular
basis at least after every six months.
REFERENCES
1.
Leff SP. Side effects of oral contraceptives:
occlusion of branch artery of the retina. Bull Sinai Hosp Detroit. 1976; 24: 227–9.
2.
Aggarwal RS, Mishra VV, Aggarwal SV. Oral contraceptive pills: A risk factor for retinal
vascular occlusion in in-vitro fertilization patients. J Hum Reprod Sci. 2013; 6: 79–81.
3.
Hayreh SS. Prevalent misconceptions about acute
retinal vascular occlusive disorders. Prog Retin Eye Res. 2005; 24: 493–519.
4.
Wang YE et al. Association between
oral contraceptive use and glaucoma in the United States. Poster presented at:
Annual Meeting of the American Academy of Ophthalmology; Nov. 17-19, 2013; New
Orleans. PO339.
5.
Kurtul BE, Inal B,
Ozer PA, Kabatas EU. Impact of oral contraceptive pills on central corneal
thickness in young women. Indian J Pharmacol. 2016;
48 (6): 665–668.
6.
Newman-Casey PA,
Talwar N, Nan B, Musch DC, Pasquale LR, Stein JD. The potential association between
postmenopausal hormone use and primary open-angle glaucoma. JAMA Ophthalmol. 2014 Mar; 132 (3): 298-303.
Doi: 10.1001/jamaophthalmol.2013.7618.
PMID: 24481323; PMCID:
PMC4106136.
7.
Scott E, Zhang QG,
Wang R, Vadlamudi R, Brann D. Estrogen neuroprotection and the critical
period hypothesis. Front Neuroendocrinol. 2012
Jan; 33 (1): 85–104.
8.
Wang YE, Kakigi C,
Barbosa D, Porco T, Chen R, Wang S et al. Oral Contraceptive Use and Prevalence of
Self-Reported Glaucoma or Ocular Hypertension in the United States. Ophthalmology. 2016 Apr; 123 (4): 729-36.
Doi: 10.1016/j.ophtha.2015.11.029. Epub 2016 Feb 11. PMID: 26948305; PMCID:
PMC4857187.
9.
Pasquale LR, Kang JH. Female reproductive factors and
primary open-angle glaucoma in the Nurses' Health Study. Eye, 2011; 25 (5): 633-641).
10.
Dong SY, Si YB, Zhang
YY, Zhao GM. Risk factors analysis of primary open angle
glaucoma in women. Zhonghua Yan Ke Za Zhi. 2013;
49: 122–5.
11.
Bhanwra S, Ahluwalia K. The association of oral contraceptive
pills with increase in intraocular pressure: Time for pharmacovigilance to step
in. J Pharmacol Pharmacother. 2015; 6: 51-2.
12. Lee AJ, Mitchell P,
Rochtchina E, Healey PR. Blue Mountains Eye
Study. Female reproductive factors and open angle glaucoma: the Blue Mountains
Eye Study. Br J Ophthalmol. 2003; 87 (11): 1324–8.
13.
Vajaranant TS,
Pasquale LR. Estrogen deficiency accelerates aging of the
optic nerve. Menopause, 2012; 19: 942-7.
14.
Burgoyne CF. A biomechanical paradigm for axonal
insult within the optic nerve head in aging and glaucoma. Exp Eye Res. 2011; 93
(2): 120–32.
15.
Harwerth RS, Wheat JL, Rangaswamy NV. Age-related losses of retinal ganglion
cells and axons. Invest Ophthalmol Vis Sci. 2008; 49 (10): 4437–43.
16.
Sung KR, Wollstein G, Bilonick RA,
Townsend KA, Ishikawa H, Kagemann L et al. Effects of age on optical coherence
tomography measurements of healthy retinal nerve fiber layer, macula, and optic
nerve head. Ophthalmology, 2009; 116 (6): 1119–24.
17.
Bayard F, Louvet JP,
Moatti JP, Smilovici W, Duguet L, Boulard C. Plasma concentrations
of LH and of sex steroids during the normal menstrual cycle and during
contraceptive treatment. J Gynecol Obstet Biol Reprod. 1975; 4: 915-26.
18. Sen E, Onaran Y,
Nalcacioglu-Yuksekkaya P, Elgin U, Ozturk F. Corneal biomechanical parameters during
pregnancy. Eur J Ophthalmol. 2014; 24: 314-9.
19. Giuffrè G, Di Rosa L, Fiorino F, Bubella
DM, Lodato G. Variations in central corneal thickness
during the menstrual cycle in women. Cornea, 2007;
26: 144–6.
20. Vajaranant TS, Maki PM, Pasquale LR, et al. Effects of
hormone therapy on intra ocular pressure: The women’s health Initiative –sight
Wxam Study. Am J Ophthalmol. 2016; 165: 115-24.